In the newly liberated regions of Ukraine, receiving a medical referral is only half the battle. For patients in remote, conflict-affected communities, the journey to specialized care can be as challenging as the health condition itself. Our experience deploying mobile health teams revealed a stark reality: even when we eliminated service costs and facilitated quality referrals, nearly half of patients still couldn’t access the care they needed.
The missing piece? Transportation.
The Problem: A 50% Gap in Healthcare Access
When we launched our integrated mobile health teams in December 2022, starting in Kharkiv oblast and rapidly expanding to Zaporizhia, Kherson, and Mykolaiv, we built what we thought was a comprehensive referral system.
Our teams— some of them comprising Ministry of Health medical personnel, psychologists, and social workers—were reaching remote communities through trusted local channels.
We mapped referral facilities across multiple categories: specialist consultations, diagnostic services, imaging, procedures, and hospitalization.
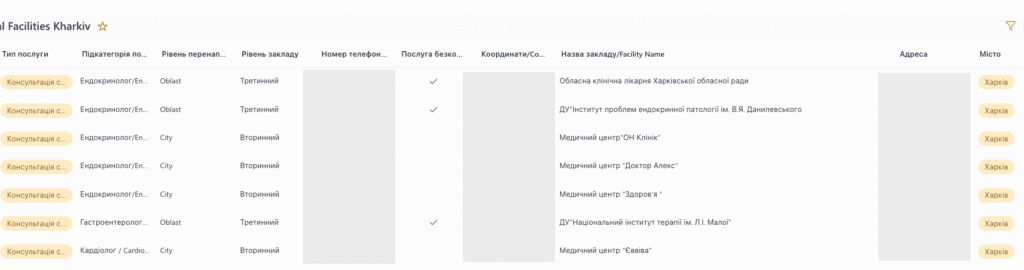
We implemented rigorous quality assurance protocols, including direct facility contact, appointment booking, and systematic follow-up.
Yet our positive referral rate stalled at 45-50%, far below our 70% target.
Diagnosing the Barrier
Through bottleneck analysis, we identified two primary obstacles preventing patients from accessing referred services:
Service costs were the first barrier. Many patients simply couldn’t afford the medical services they needed, even when clinically necessary. Our solution was to integrate with the Ukrainian’s government Medical
Information System (MIS) to facilitate e-referrals, channeling patients through the medical guarantees program that covers service costs. We automated the process through SharePoint Lists and Power Automate, creating a seamless workflow from our mobile teams to government coverage.
The results were encouraging—positive referral rates climbed to 58-60% for e-referrals. But that still left 40% of patients unable to access care, even when services were completely free.
Transportation costs emerged as the persistent, critical barrier. In remote, conflict-affected areas, public transportation is often nonexistent. Private transportation comes at a cost many families cannot bear, particularly when facing the compounding pressures of displacement, loss of income, and ongoing insecurity.
The Solution: Cash for Medical Transportation
Understanding that financial barriers required financial solutions, we developed a targeted cash transfer program specifically for medical transportation. The program was designed with several key principles:
Evidence-Based Calculations
Rather than arbitrary amounts, we built a distance-based calculation model:
- Assumption: 12 liters of fuel per 100 kilometers
- Costs factored: fuel, vehicle amortization, maintenance, plus a 10-15% buffer
- Coverage: round-trip transportation for the patient
- Maximum payment: 1,800 hryvnias (~$45 USD)
- Average payment: 1,100 hryvnias (~$27 USD)
We created a living matrix based on beneficiary location and referral site distance, updated every six months to reflect fuel price fluctuations.
Clear Eligibility Framework
Inclusion criteria focused on patients with clinically sound, evidence-based referrals that didn’t require regular, frequent visits—ensuring we addressed acute access barriers without creating long-term dependency.
Exclusion criteria prevented mission creep: no support for medicine procurement or ongoing treatments requiring weekly or monthly visits. Patients could receive cash support only once every six months, with rare exceptions.
Secure Transfer Modalities
We prioritized accountability through formal transfer channels—bank transfers or UkrPoshta (postal service)—rather than cash-in-hand. While this added a 1.5-month lead time, it ensured traceability and reduced risks.
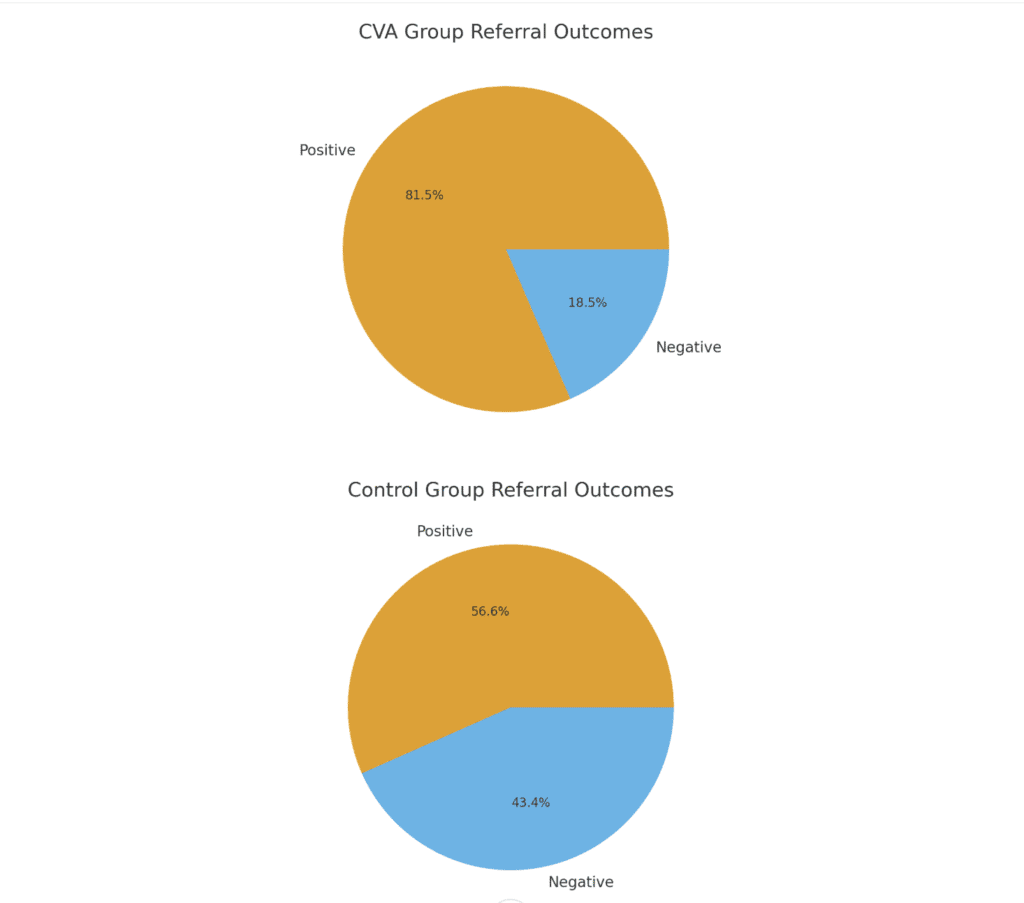
The Results: A 30-Point Increase in Access
The impact was clear and consistent. You can dive into the numbers in the page dedicated to the program analysis.
With cash support:
- E-referrals: 80-82% positive referral rate
- Standard referrals: 78% positive referral rate
Without cash support (control group):
- E-referrals: 58% positive referral rate
- Standard referrals: 55% positive referral rate
Cash for medical transportation increased successful referral completion by approximately 25-30 percentage points. Critically, it worked across both groups, whether or not service costs were covered through e-referrals. This confirmed that transportation represents an independent, addressable barrier to healthcare access.
Lessons Learned: Continuous Improvement
No program is perfect from launch. As we’ve scaled, we’ve identified areas for improvement:
Multi-Tiered Communication
UkrPoshta cash delivery, while secure, isn’t foolproof. SMS notifications fail, patients don’t answer calls, or network coverage is spotty. We developed a three-tiered follow-up protocol:
- Plan A: Direct contact from nurses and doctors;
- Plan B: Community health workers provide in-person notification, leveraging local trust and presence.
- Plan C: potential Viber or a text messaging upon the transfer of cash.
This approach ensures accountability to affected populations even when standard channels fail.
Enhanced Data Collection
We currently lack systematic data on negative referrals where cash support was provided. Understanding why patients who received funds still didn’t access services is critical for continued improvement. We’re exploring ways to shift this data collection to office staff, reducing the burden on our mobile teams whose capacity is fully occupied with clinical duties.
Statistical Rigor
While our trends are encouraging, we’re working to strengthen our analytical foundation with larger sample sizes and longer observation periods to draw more definitive conclusions about program effectiveness.
Implications for the Humanitarian Response
Our experience offers several insights for humanitarian actors working in conflict-affected settings:
1. Multifaceted barriers require multifaceted solutions. Healthcare access isn’t just about clinical capacity or service availability. Financial barriers—both service costs and transportation costs—can independently prevent care access. Comprehensive programs must address all three.
2. Cash transfers are effective tools in health programming. While often associated with food security or livelihoods, well-designed cash interventions can directly improve health outcomes by removing financial barriers to care-seeking.
3. Digital systems enable accountability and learning. Our transition from Excel sheets to SharePoint Lists with Power Automate wasn’t just about efficiency—it enabled systematic tracking, follow-up, and evidence generation that informed program adaptation.
4. Integration with government systems amplifies impact. By connecting our mobile health teams to Ukraine’s MIS system through e-referrals, we leveraged existing resources and ensured sustainability beyond our direct intervention.
5. Local engagement strengthens last-mile delivery. Community health workers proved essential for ensuring cash notifications reached beneficiaries when formal systems failed—a reminder that humanitarian innovation must include, not replace, community-based approaches.
Looking Ahead
As we continue refining this model, we’re exploring how to support patients who need more frequent access to referred services—those with ongoing treatments requiring monthly or bi-weekly visits. Can we integrate with public transportation systems where they exist? Should we consider recurring compensation models for chronic conditions? These questions will shape the next evolution of our approach.
The conflict in Ukraine has created immense healthcare challenges, particularly in newly liberated areas where infrastructure has been damaged or destroyed. But it has also created space for innovation—for testing models that combine humanitarian cash programming with health system strengthening in ways that could have applications far beyond Ukraine.
Transportation may seem like a mundane barrier compared to the dramatic challenges of conflict-affected healthcare delivery. But for the 78-82% of patients who now successfully access referred services—up from just 50% before cash support—that journey to care has become possible.
Sometimes breaking barriers is about building roads. Sometimes it’s about removing the financial obstacles standing in the way of the roads that already exist.

Leave a Reply